http://www.dallasheart.com/resources/AFib.pdf
ANTI-ARRHYTHMICS
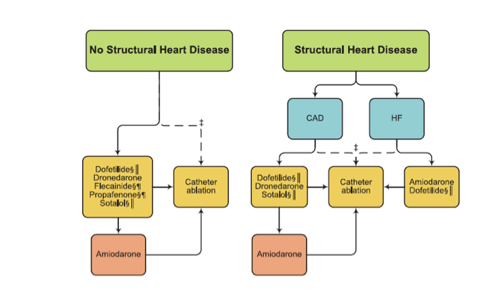
Class I: “Because of its potential toxicities, amiodarone should only be used after consideration of risks and when other agents have failed or are contraindicated”
(ACC/ AHA Guidelines on AFib Circulation 2014; 130: e230)
***FLECAINIDE NOTES****
Uses:
-Atrial Fibrillation / Atrial flutter
-PVCs
Contra-indications
-Coronary Artery Disease (CAST Trial)
-Structural Heart Disease
-LVH > 1.4 cm
-Reduced LVEF
Toxicities:
-Use Dependent --> Follow QRS during treadmill after initiation
*****SOTALOL NOTES********
-Reverse Use Dependent Effects --> Best to measure QTc during sinus rhythm
-Most effective (and toxic) at lower heart rates (reverse use dependent effects)
-If they have a Left Bundle Branch Block or Ventricular Paced Rhythm --> can consider using JTc
*****DOFETILIDE NOTES*******
Please go to this page: http://dallasheart.com/page2/page82/page82.html
SAMPLE AFIB WORKSHEET:
HPI:
Document the Following:
-History of CAD / MI / PCI / CABG?
-If so, list what symptoms they presented with (CP? SOB?) , what hospital they went to, what work did they have (TTE? Cath?)
-History of Afib:
-How did they present? How was it diagnosed?
-What symptoms do they have from Afib? (LH/dizziness, palpitations, racing heart rate sensation, syncope, pre-syncope, chest pain, dyspnea, fatigue, CHF etc)
-How were they treated? (Ever have a DCCV? Placed on any AAD or anticoagulation?)
ASSESSMENT & PLAN:
1. (Put classification of Afib here) Atrial Fibrillation:
-The patient has new onset (or diagnosis) AFib / Paroxysmal / Persistent / Long Standing Persistent / Permanent AFib (recurrent?)
-Initial diagnosis was _______
-Patient is asymptomatic / symptomatic with his/her Atrial fibrillation (list symptoms here)
-Patient’s time line is as follows: (starting from initial diagnosis, list times and dates of DCCVs, history of AAD, and AFib ablations)
-In regards to anticoagulation, the patient’s CHADS2-VASc score is ____